The main reason to get boosted: reducing the chances/severity of long COVID; How much does the new booster reduce your chances of getting COVID?; What about myo/pericarditis, especially for young men?
I continue to follow COVID developments, but not as closely anymore because, as I have been writing since as far back as December 14, the pandemic has become endemic.
Below is what I sent to my coronavirus e-mail list yesterday. To sign up for it, simply send a blank e-mail to: cv-subscribe@mailer.kasecapital.com.
1) In my last e-mail on Wednesday, I shared the fact that I got my second COVID booster the day before and shared the reasons for my decision. One of them was that getting sick again increases my chances of long COVID.
I want to discuss this further because this is the most important reason I decided to get a second booster...
I'm not worried about the short-term sickness, which is nearly certain to be no worse than a few days of flu-like symptoms, given my age, excellent health, and experience getting COVID last December.
Nor does getting a booster dramatically reduce my chance of getting COVID (see discussion below).
But I'm really spooked by long COVID for a few reasons:
- There doesn't appear to be any pattern regarding who gets long COVID and the symptoms/severity (see: The Mysteries of Long COVID). I don't like this uncertainty one bit...
- It's alarmingly common: Data from the CDC shows that nearly 15% of Americans who've gotten COVID are "reporting symptoms lasting three months or longer reduced ability to carry out day-to-day activities..." A study in Scotland "found that one in 20 people who had been sick with COVID reported not recovering at all, and another four in 10 said they had not fully recovered from their infections many months later." Another showed that, globally, 1% of COVID patients have persistent symptoms after a year (see: Long COVID Disables Millions Worldwide, Even as Rates Ease, Study Shows).
- Long COVID symptoms are extremely serious, including fatigue, brain fog, respiratory issues, body-wracking tremors, and debilitating migraine headaches. Given the history of dementia in my family, the last thing I need is anything that could trigger this or speed it up (see: Possible 69% higher risk of Alzheimer's for older COVID survivors). And it's possible that getting COVID is what caused my dad's A-fib (he's back in Kenya and his A-fib is fine, though he just got COVID for the second time – very mild symptoms, however).
This is what my cousin posted on Facebook six weeks ago:
I've debated posting anything about this because I don't know what good it would do, but here goes.
I have Long COVID.
On August 14th I tested positive and had brief fever and chest congestion. But in the weeks that followed my days have been met with excruciating exhaustion, nausea, brain fog, and body aches. It started when I tried to go for a walk and almost passed out after barely two blocks. For about two weeks my appetite cratered, I could hardly tolerate most solid food without vomiting, and I lost about 30 pounds.
It's been two months and things have improved enough for me to be able to go back to work, but planning any kind of social outing is difficult. I don't know how much energy I'll have, or how much pain I'll be in on any given day. I'm told that people eventually get better and every doctor I've seen has said the same thing, but it will probably be weeks or months before I truly feel like myself again.
In spite of everything, I feel lucky to be alive even on the bad days.
If you have gotten this far, thank you for reading. If you are experiencing/have experienced long COVID and need an ear, my DMs are open.
So is there evidence that people who are vaccinated and/or boosted are less likely to get long COVID?
Yes, though (as with just about everything related to it) the evidence isn't perfect. This Bloomberg article, Will Vaccines Protect Me From Long COVID?, notes:
They can also reduce the chance you'll become severely ill if you're infected, which also makes long COVID less likely, Justman says.
A few published studies have suggested long COVID occurs less frequently among those who had COVID after being vaccinated. At least one study has shown rates of long COVID decreasing with every additional round of shots. But there is a lot of work left to understand the illness. And vaccines don't offer perfect protection.
"This is where the roll of the dice comes into play," Justman says.
And the Scotland study cited above found:
... vaccination appeared to help reduce if not eliminate the risk of some long COVID symptoms.
People with severe initial COVID cases were at higher risk of long-term problems, the study found.
2) One of my friends (who tends to be a vaccine skeptic) points to my dad (who just got COVID despite five shots) and his own experience (everyone in his family got COVID despite being vaccinated) as proof that the vaccinations/boosters don't reduce your chances of getting COVID (rather, their only benefit is reducing illness among those who get it).
This is certainly contrary to everything I've read, so I did some digging and discovered that the CDC just released a new study on November 22 addressing this very question: Effectiveness of Bivalent mRNA Vaccines in Preventing Symptomatic SARS-CoV-2 Infection. It studied 360,626 Americans covering every possibility: every age 18 and up; 34% had COVID, the balance didn't; 28% were unvaccinated, the balance had various levels of vaccination.
Here's the summary of the report's finding:
In this study of vaccine effectiveness of the U.S.-authorized bivalent mRNA booster formulations, bivalent boosters provided significant additional protection against symptomatic SARS-CoV-2 infection in persons who had previously received 2, 3, or 4 monovalent vaccine doses. Due to waning immunity of monovalent doses, the benefit of the bivalent booster increased with time since receipt of the most recent monovalent vaccine dose.
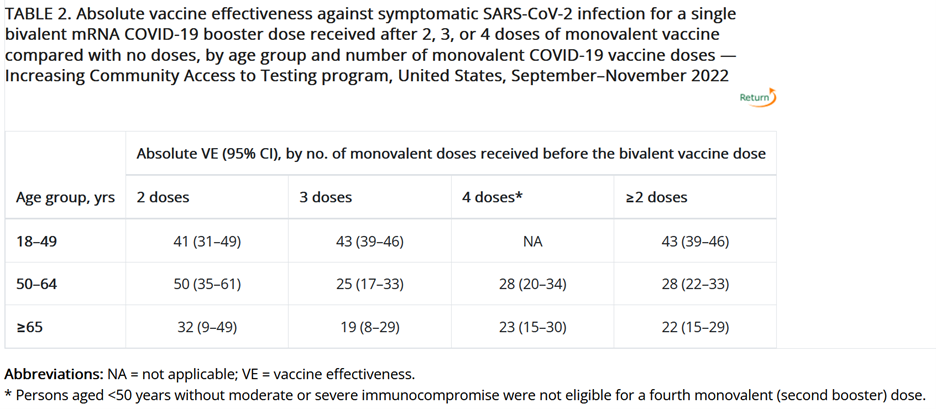
And here is the key table:
So for me (age 56 with three prior doses), the study showed that the vaccine effectiveness ("VE") was 25%. For my dad (age 80 with four prior doses), the VE is 32%.
However, the VE is much higher for people who haven't had a shot/booster in eight or more months, as this more in-depth table shows:
So for me, given that my last dose was 13 months ago (and my only bout with COVID was 11 months ago), the VE is at least double: 51%.
Dr. Kevin Maki commented:
The results show only modest incremental protection against symptomatic COVID. And keep in mind that these results are short term, since the bivalent booster has only been out for a few weeks. One would expect the protection against symptomatic infection to fade with time, so the incremental protection against symptomatic COVID over a full six-month cold/flu/COVID season is probably smaller. I expect that the main benefit will be to reduce severity of symptoms when an infection occurs (a substantial benefit).
I would also add that the study didn't say anything about adverse effects, nor whether just giving people the old monovalent booster would have worked just as well.
But it clearly says that most people get a decent reduction in the chances of getting COVID (generally 30% to 50%, depending on age and date of previous shot – roughly in line with the effectiveness of the annual flu shots).
While those numbers aren't nearly as good as the 90%-plus reduction that the original vaccines provided against the old COVID variants, they're still quite good.
My conclusion: Getting a booster provides a modest benefit regarding not getting COVID, continued large protection in mitigating serious illness, and an unknown but possibly substantial reduction in the chances/severity of long COVID.
That's why I'm very happy that I got boosted last week, especially given my heavy travel schedule in December and January and that it had been 13 months since my last shot and 11 months since I'd had COVID.
3) My friend also argued that, given the risks of the vaccination causing myo- and pericarditis, it didn't make sense for most people to get an additional shot.
To address this nuanced question, I turned to Dr. Maki, who wrote:
My reading of the totality of the literature suggests that COVID does increase myo/pericarditis risk, although estimates have varied by study, with some showing no increase. Also, this study "found that full vaccination against COVID-19 was associated with a reduced risk of acute myocardial infarction and ischemic stroke after COVID-19."
The greatest risk seems to be in males under 30 years of age, which is a group for which the risk/benefit ratio for vaccination and boosting is uncertain from my perspective – see this study, which concluded:
Results of this large cohort study indicated that both first and second doses of mRNA vaccines were associated with increased risk of myocarditis and pericarditis. For individuals receiving 2 doses of the same vaccine, risk of myocarditis was highest among young males (aged 16-24 years) after the second dose. These findings are compatible with between 4 and 7 excess events in 28 days per 100,000 vaccinees after BNT162b2, and between 9 and 28 excess events per 100,000 vaccinees after mRNA-1273. This risk should be balanced against the benefits of protecting against severe COVID-19 disease.
Some countries do not allow vaccination of men under 30 years because of this concern.
I really wish the NIH would fund studies in this subgroup at highest risk for myocarditis to compare vaccines and evaluate the risk with boosters. The J&J vaccine might be a good option, although I think two doses are needed to get reasonable protection. Novavax may be a good option, although there are reports of myocarditis with the second injection, which is an adjuvant intended to enhance the immune response. Currently, we are flying more blind than I would like.
The estimate of benefit vs. risk for boosting is therefore dependent on several variables: age, comorbidities, sex, recency of prior vaccination or infection with COVID, and history with prior vaccinations.
I have a friend who is a cardiologist. He has taken all of the boosters but his wife has a history of pericarditis, which flared with the second dose of mRNA vaccine. She received a J&J booster without incident but that is no longer readily available. Accordingly, after consulting with several experts, they decided that she would not get boosted again.
So... we have reached a point where I think that people should have a discussion with a healthcare professional about risks and benefits so that they make truly informed decisions about boosting.
For those aged 60 and up, the ratio will likely be favorable for most of the population as the benefit of reducing severity of COVID probably outweighs the risk of myo/pericarditis for boosting, although we need more real-world data to better estimate magnitudes.
As for young men, I think that for a male 16-24 years of age without significant comorbidities who has previously had COVID, vaccination is probably not justified by the potential benefit, weighed against the potential risk. However, that rests on several assumptions about risk of reinfection, potential for long COVID, risk of severe outcomes with Omicron subvariants, etc., so reasonable people with the proper expertise might disagree with this viewpoint!
The story is also mixed for most youth. Denmark is stopping vaccination of those under 18 years, in the absence of "a specific medical assessment," because their health authorities do not believe that the risk/benefit ratio is favorable. Given the high level of immune resistance in the population, the low rates of hospitalization for kids, and the risk for myocarditis in males, I believe that approach is defensible, although I favor a more nuanced, case-by-case approach that would take into account gender, risk factors, prior infection status, etc. I think vaccinations should now be available in physician offices, which facilitates a discussion between doctor/parent/patient.
As for me, I was originally planning to get the bivalent booster before my trip to Morocco, but a hurricane derailed that. Then I got the flu (four weeks after my flu vaccine), so I will get boosted next month. I appear to be one of the roughly 6% of Americans that has not had COVID based on many antibody tests I have taken roughly monthly. Same for my 22-year-old son. Not true for my wife and daughter. That might be good luck or it might be that my son and I have immune resistance for some unknown reason.
Thank you, Dr. Maki!
Best regards,
Whitney
P.S. I welcome your feedback at WTDfeedback@empirefinancialresearch.com.